In the field of tumor diagnosis and treatment, MRD (Minimal Residual Disease) testing is playing an increasingly important role, providing key evidence for evaluating treatment efficacy and predicting recurrence risk [1-3]. However, testing costs often reaching tens of thousands of yuan, along with subsequent monitoring costs of several thousand yuan per session, often deter researchers and patients.
In this article, let's delve into the mysteries behind MRD testing prices and explore how to balance cost and effectiveness.
MRD testing process (this article mainly discusses the Tumor-informed ctDNA MRD testing process)

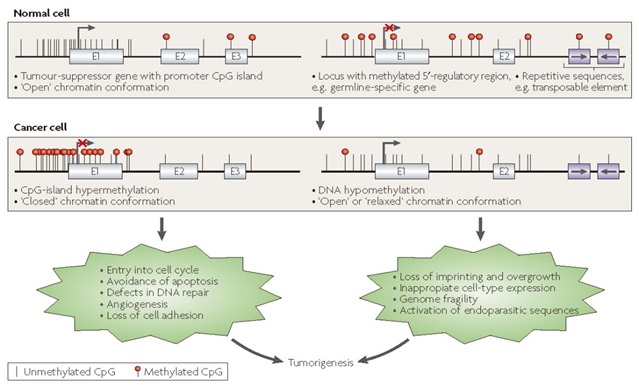
Figure 1. Overview of MRD Detection [4]
Price Difference Point 1: WES-based initial screening involves large data volume and high cost
In the Tumor-informed detection strategy, obtaining a sufficient number of patient-specific loci through WES initial screening and selecting the number of loci for monitoring in each patient is also crucial for the sensitivity of subsequent MRD detection.
The 2025 CSCO Colorectal Cancer Diagnosis and Treatment Guidelines added ctDNA MRD to the Level III recommendations for postoperative follow-up of colorectal cancer. Regarding the selection of ctDNA MRD technology, it preferentially recommends personalized ctDNA mutation detection technology based on WES-based tumor-informed analysis [5]. In MRD detection, the somatic loci screened vary among different cancer types, with a median TMB of 3.6 mutations/Mb. Screening with a ~2 Mb large tumor panel yields approximately 7 loci, while screening with a ~35 Mb whole exome significantly increases the number to approximately 126 loci. The more traceable gene mutations detected, the higher the sensitivity of subsequent blood MRD monitoring, and the better the detection performance for samples with low initial amounts.
However, the sequencing cost of whole exome sequencing is very high.
For detecting low-frequency somatic mutations, tumor genes typically require a deduplicated depth of up to 500× to ensure the accuracy of detection. For conventional whole exome products on the market, this corresponds to a data volume of approximately 50 Gb, plus 10 Gb for control samples, resulting in a total data volume of about 60 Gb per sample. The cost for a single sequencing of one sample can be as high as 1,200 RMB (estimated at 20 RMB/Gb), which is significantly higher than that of conventional detection products relative to general reagent prices.
In response, the AIExome-V5 Tumor can effectively save up to 30 Gb of data volume, reducing initial screening costs by at least 50%.
Feature 1: High hotspot depth
The AIExome-V5 Tumor, with its unique depth-differentiated adjustment technology, achieves a depth in tumor-related regions that is significantly ~4 times higher than that in other exome regions. That is, with 10 Gb of data, when the average depth of the whole exome region is 100×, the depth of tumor-related genes can reach approximately 400×. This enables accurate detection of low-frequency somatic mutations related to tumors in whole exome sequencing even with low data volume.

Figure 2. Depth ratio statistics of different probe panel regions in AIExome-V5 Tumor.
Feature 2: Comprehensive variant detection
On the basis of comprehensively covering the protein-coding regions of the entire genome, it additionally includes detection regions for Fusion, MSI, HLA, HRD, and mtDNA. This enables one tube of probes and one detection run to comprehensively meet various variant detection needs, truly achieving All-in-one.

Figure 3. Coverage of CDS regions in various databases: AIExome V5 vs. competitors. *RefSeq & refGene: the union of CDS from the latest RefSeq and refGene; RefSeq version is v20240129, refGene version is 20200817
Feature 3: Short detection cycle
To meet the demand for ultra-fast cycle detection, it has been upgraded to the DNA probe version of whole exome, making it easier to use. Equipped with v3.0 hybridization capture reagents, it can meet users' needs with high standards whether for overnight hybridization or fast hybridization.

Figure 4. Capture performance of AIExome V5 Tumor probes paired with TargetSeq one v3.0 (fast hybridization and overnight hybridization).
Feature 4: Accurate mutation detection
While saving data volume and increasing depth, the high-depth tumor-related regions enable accurate detection of low-frequency mutations.
Table 1. Statistics of mutation detection in positive standards

Price Difference Point 2: High cost of personalized customized MRD Panels
2.1 In the customization process of MRD Panels, custom probes from column-based synthesis manufacturers are commonly used. Considering that the number of customized loci directly affects the cost, the number of loci is generally controlled between 10-30. Even so, it will still incur a customization cost of approximately 1,500 RMB per patient, and fewer loci will also have an adverse impact on subsequent MRD detection.
In response, IGT has launched a free MRD customization scheme where each Panel can include up to 150 probes (approximately 150 loci). While significantly increasing the number of traceable loci to improve detection results, it achieves zero-cost customization for each patient.
2.2 In the entire chain of MRD testing, to ensure highly efficient reagent performance in every link for achieving sensitive and accurate detection, there is more to choose from than just expensive foreign reagents.
After years of independent research and development of supporting reagents and expansion of applications in various scenarios, iGeneTech has formed a complete solution covering sample extraction, library preparation, capture, and bioinformatics analysis. The performance of its library preparation and capture reagents is not inferior to that of foreign competitors. Meanwhile, each link can be stably and efficiently used with automated equipment, enhancing the high cost-effectiveness of reagents throughout the entire detection process.
2.3 To achieve a sequencing depth of 100,000× for each test, smaller Panels have lower data utilization rates, requiring larger data volumes and thus higher sequencing costs.
IGT achieves a capture efficiency of ≥ 50% for 15–150 probes. For a Panel with approximately 30 loci, only about 1 Gb of data volume is needed to reach an ultra-high sequencing depth of around 180,000×, meeting the needs of subsequent ultra-low abundance detection.
Figure 6. Statistical results of MRD Panel tests with different numbers of probes. Based on IGT's overall MRD Panel solution, 33 synthesized different MRD Panels (containing 15–150 loci) were statistically tested for capture performance.
Individually customized Panels with different monitoring loci obtained from initial screening can be formed in one go and used stably and efficiently. Even small Panels with only 15 probes, when combined with IGT's capture system, can still maintain a capture efficiency of over 60%.
Summary
AIExome V5 Tumor, paired with free customization of Tumor-informed MRD, comprehensively screens monitoring loci. High-quality reagents throughout the entire process ensure detection results, greatly reducing the customization and reagent costs of MRD testing. This helps every tumor patient benefit from the clinical value brought by MRD testing.
References
[1]. Jacqueline A, Shaw,Karen, Page,Evie, Wren et al. Serial Postoperative Circulating Tumor DNA Assessment Has Strong Prognostic Value During Long-Term Follow-Up in Patients With Breast Cancer.[J] .JCO Precis Oncol, 2024, 8: 0.
[2]. Yin, Yang,Tao, Zhang,Jingbo, Wang et al. The clinical utility of dynamic ctDNA monitoring in inoperable localized NSCLC patients.[J] .Mol Cancer, 2022, 21: 0.
[3]. Song, Dong,Zhen, Wang,Jia-Tao, Zhang et al. Circulating Tumor DNA-Guided De-Escalation Targeted Therapy for Advanced Non-Small Cell Lung Cancer: A Nonrandomized Controlled Trial.[J] .JAMA Oncol, 2024, 10: 0
[4]. rsons H A , Rhoades J , Reed S C , et al. Sensitive Detection of MinimalResidual Disease in Patients Treated for Early-Stage Breast Cancer[J]. ClinicalCancer Research, 2020, 26(11):clincanres.3005.2019.
[5]. CSCO结直肠癌诊疗指南(2025版)
[6]. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Medicine (2017) 9:34

 CN
CN